While some pediatric endocrine disorders can be easily diagnosed, others may be trickier to detect. Common pediatric endocrine disorders include short stature, Turner syndrome, type 1 diabetes, and thyroid disorders.
Often, these disorders may impact linear growth, behavior, cognition or school performance, energy levels, and/or hasten or delay pubertal development. For these reasons, it is important to diagnose pediatric endocrine disorders early on and start treatment promptly.
In this blog, we will discuss the signs, symptoms, and treatments for common pediatric endocrine disorders.
Short Stature and Abnormal Linear Growth

Short stature can be defined as being less than the third percentile on the growth curve or significant short stature as below the first percentile. Abnormal linear growth happens when a child starts crossing growth percentiles. The latter is most concerning, but both should be given some thought and evaluation.
Evaluating & Treating Short Stature
An evaluation would include a medical provider asking specific questions related to general health, obtaining family history, familial heights, current medications, and performing a thorough physical exam. A bone age is determined with an x-ray of the left hand looking at growth plates and bone maturation. Blood work might also be warranted to look for an etiology.
Qualifying children may be eligible for treatment with recombinant growth hormone injections. These children will often be referred to a Pediatric Endocrinologist for further evaluation and initiation of growth hormone therapy. Extremely short children benefit most from growth hormone therapy when it’s initiated early and before they start puberty.
Turner Syndrome
Turner syndrome is a genetic condition where girls are missing an X chromosome in some or most of the cells. Turner syndrome can be suspected in utero on a prenatal ultrasound, soon after birth or during adolescense if physical signs are subtle. Prenatal genetic testing can aid in early diagnosis.

Signs of Turner Syndrome
Some signs and symptoms of Turner syndrome include:
- Puffy hands and feet
- Wide neck
- Slowed growth/short stature
- Heart malformation
- Delayed puberty
- Abnormal kidneys
Diagnosis and Treatment of Turner Syndrome
Often the primary care team will order a karyotype to confirm the diagnosis. After the diagnosis is made, many tests and studies, if not already done, are conducted to look for associated features.
Treatment will depend on the findings of the tests and studies. A pediatric endocrinologist is often an essential member of the care team for children with Turner syndrome. In fact, a pediatric endocrinologist may see your child more often than her primary care provider.
Girls with Turner syndrome see a pediatric endocrinologist specifically for slowed growth or pubertal delays and autoimmune diseases such as hypothyroidism, hyperthyroidism, or type 1 diabetes. As slowed growth becomes obvious, often recombinant growth hormone is initiated to improve adult height outcomes. It is beneficial to start treatment as soon as slowed growth is observed to get the maximum benefit from growth hormone.
Another aspect of treatment provided by a pediatric endocrinologist is pubertal initiation. More often than not, girls with Turner syndrome do not start puberty. Not only is estrogen vital for bone health, cardiovascular health, and the adolescent growth spurt, it is important for these girls to experience similar changes seen in puberty as their peers.
Type 1 Diabetes

Type 1 Diabetes is an autoimmune condition in which the immune system destroys the cells that make insulin. Insulin is a hormone that allows the cells in the body to use glucose as a fuel source. Without insulin, glucose levels are high in the bloodstream and in the urine. The body starts to use fat as energy alternatively leading to the build of ketones in the bloodstream and urine that worsen the severity of the illness.
Signs of Type 1 Diabetes
Some signs and symptoms of Type 1 diabetes include:
- Weight loss
- Nausea/vomiting
- Thirst
- Abdominal pain
- Frequent urination
- Vision changes
- Hunger
- Fatigue
Diagnosis & Treatment of Type 1 Diabetes
The diagnosis of type 1 diabetes is made from blood work. Elevated blood glucose levels are noted and there may also be presence of ketone bodies in the blood and urine. Antibody levels are often measured to confirm the diagnosis of type 1 diabetes.
The treatment involves prompt initiation of insulin injection therapy. Soon after the child is diagnosed with type 1 diabetes, a pediatric endocrinologist is consulted. Moreover, the pediatric endocrinologist will make recommendations on insulin therapy and doses. The family and child are taught how to manage diabetes at home.
Your child may also be a candidate for immunotherapy to delay the onset of Type 1 Diabetes.
The child will see the pediatric endocrinologist every 3 months or more frequently if needed. If the diagnosis is delayed, the child may present severely ill and require admission to the intensive care unit and placed on intravenous insulin.
Graves' Disease
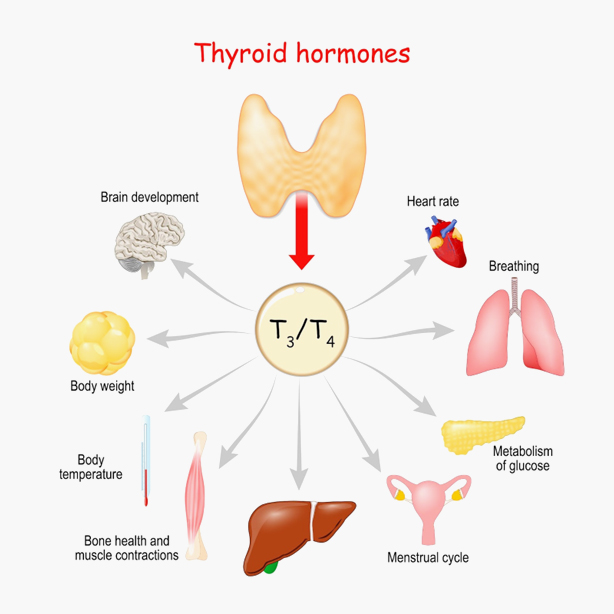
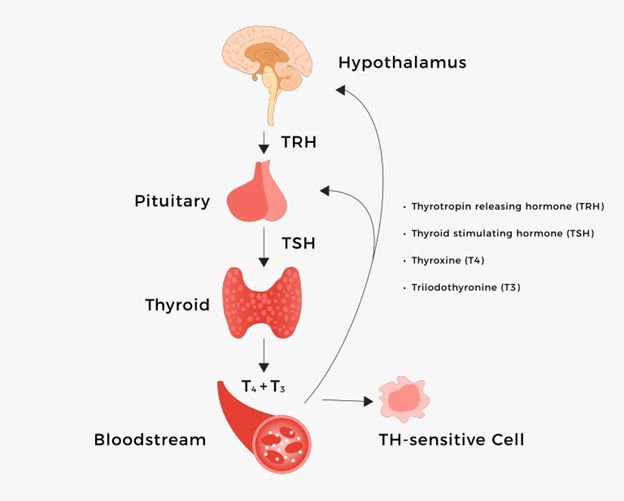
Graves' disease is an autoimmune disease that leads to an overactive thyroid gland or hyperthyroidism. It is the most common cause of hyperthyroidism in children.
Signs of Graves' Disease
Here are some signs and symptoms of Graves' disease:
- Enlarged thyroid gland
- Difficulty sleeping
- Bulging eyes
- Weight loss
- Poor school performance
- Menstrual irregularities
- Fidgeting
- Nervousness
- Increased appetite
- High heart rate
Diagnosis & Treatment of Graves' Disease
For Graves' Disease, the diagnosis is made by evaluating thyroid hormone levels in the blood. There are several treatment options available after discussion with your pediatric endocrinologist based on the clinical findings and the age of the child.
A common therapy is to give medication that lowers the thyroid hormones that are released from the thyroid gland. The other option is to give radioactive iodine to ablate or destroy the gland. Some individuals might be better suited for surgical removal of the thyroid gland.
Early diagnosis and treatment are important to help the child feel better, grow normally, and improve school performance if impacted.
Hashimoto’s Thyroiditis
Hashimoto’s thyroiditis is an autoimmune condition that can lead to hypothyroidism or an under active thyroid gland. It is the most common cause of hypothyroidism.
In this condition, the immune system destroys the thyroid gland. During this immune dysregulation, there may be a transient hyperthyroid phase as thyroid hormone is released freely. Some individuals will end up needing thyroid hormone replacement.
Signs of Hashimoto's Thyroiditis

Here are some signs of Hashimoto’s hypothyroidism:
- Goiter
- Delayed puberty
- Slowed growth
- Constipation
- Decreased heart rate
- Fatigue
Diagnosis & Treatment of Hashimoto's
In order to diagnose Hashimoto's, obtaining blood levels of thyroid hormones is necessary.
Pediatric endocrinologists often are consulted to manage a child with hypothyroidism. Usually, treatment involves providing thyroid hormone tablets. It is important to treat hypothyroidism early to help the child feel better, grow normally, and normalize metabolism.
Congenital Hypothyroidism
Congenital hypothyroidism is a condition where a baby has hypothyroidism or under active thyroid gland. In most cases, it arises from an abnormal formation or lack of formation of the thyroid gland.
In the United States, neonates are diagnosed based on mandated newborn screening. This is because most infants are not symptomatic, and treatment prevents neurocognitive delays.
Signs of Congenital Hypothyroidism

While most infants tend not to show symptoms, here are some signs and symptoms of congenital hypothyroidism:
- Constipation
- Enlarged tongue
- Slow growth
- Prolonged jaundice
- Low heart rate
- Poor feeding
- Low body temperature
Diagnosis and Treatment of Congenital Hypothyroidism
Infants who are diagnosed by newborn screening methods will have confirmatory blood work. They will often be referred to a pediatric endocrinologist for ongoing management. It is very important to start treatment and normalize thyroid hormone levels, so the infant’s brain development is not harmed.
Find the Right Pediatric Endocrinologist for Your Child
These disorders, if left untreated, can have serious long-term consequences for a child's growth and development. However, with early detection and proper treatment, many children with endocrine disorders can lead healthy and normal lives.
It is crucial for parents and healthcare providers to be aware of the signs and symptoms of these disorders and to seek medical attention promptly if they suspect their child may be affected. By working together, we can ensure that every child receives the best possible care and support for their endocrine health.
For more information about pediatric endocrine disorders and how to get the best treatment, follow our blog or contact Dr. McIver.